
Resilient. Transforming Health Infrastructure Beyond 2020
By Dr. Hem Dholakia
Health infrastructure is the backbone of an accessible, affordable and equitable health care system. Therefore, the quality and reach of health infrastructure is a strong determinant of health outcomes. In a world where the frequency and intensity of disasters are on the rise, designing resilient health infrastructure is central to the health of nations.
In developing countries, it is often observed that there remain gaps between the demand and availability of health infrastructure. Further, though physical infrastructure may be present, health centres may be not be functioning optimally (due to lack of medical professionals, equipment, electricity, water, availability of medicines, etc.). This adds to the gap in provision of health care.
In disaster situations, these gaps are often exacerbated. A large influx of injured persons coupled with the potential destruction of physical infrastructure increases the pressures on providing timely care to save lives. The figure below shows that health infrastructure is needed at every stage of the disaster process.
Role of the Healthcare System through the Disaster Process
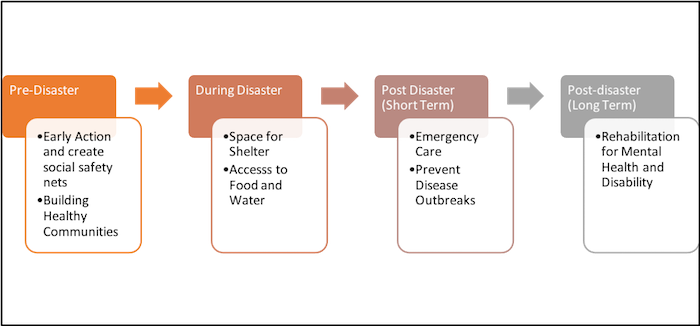
Prior to the occurrence of disasters, it plays a role in building healthy communities and laying the foundation for early action. Healthy communities can better withstand disasters. During a disaster, resilient health infrastructure can provide shelter and access to emergency care. In the post-disaster period, it can provide rehabilitation for disability or mental health issues, both of which often manifest in the long term.
It is important to note that health infrastructure should not be thought of as buildings, medicines, equipment, human resources and services alone. It needs to include supplementary infrastructure such as access roads, telecommunication systems, mobile health units and electricity. Good roads allow for speedy transportation of people to a health facility. Reliable electricity allows for continuous functioning of medical equipment. Robust communication systems allow for timely exchange of critical information and aids in decision making. Even if one part fails, it can have domino effects on other infrastructure systems. As a result, experts suggest that we adopt a 'systems approach' when thinking about resilient infrastructure.
A 'systems approach' can be thought of as a jigsaw puzzle. Each piece is intricately connected to the other. Only when all the pieces are in place is the picture complete.
Similarly, there are several pieces required to make health infrastructure resilient. Some of these pieces include an awareness of potential disasters (i.e., identification of risks); having clear rules or procedures to follow before, during and after a disaster (i.e., governance); ensuring availability of trained personnel to undertake action (capacity building); having resources to implement plans (i.e., finance); and a strong participation of people for whom the infrastructure is built (i.e., community involvement). Bringing all these pieces together is complex, but essential.
COVID-19 has exposed how fragile our health infrastructure is. However, it also offers lessons and space for poignant reflection to reimagine healthcare. The resilience of healthcare infrastructure and the resilience of societies are two sides of the same coin. As we transform healthcare infrastructure post 2020, there should be only one mantra to guide us. Resilient.
Dr. Hem Dholakia is a Lead Specialist at the Coalition for Disaster Resilient Infrastructure (CDRI)
The views and opinions expressed in this blog are those of the author and do not necessarily reflect those of the Coalition for Disaster Resilient Infrastructure (CDRI).




.jpg)

.jpg)


